Background
CBT is the typical treatment for PTSD, though outcome meta-analyses suggest 33% of traumatized clients are excluded from treatment studies due to substance use, suicidality or other “serious comorbidity”1 which may commonly co-occur with PTSD3 . DBT has been shown to effectively treat those with BPD, who often have complex trauma 4 or presenting symptomatology that mirrors the emotional distress, negative interpersonal attributions, and self-destructive behaviors (i.e. substance abuse, suicidality) in PTSD; approximately 50% of BPD clients are diagnosed with PTSD 3. DBT-PTSD, a modified DBT program with complex PTSD interventions, was shown to successfully treat PTSD with or without BPD in adult survivors of CSA 2, yet further study of DBT effectiveness on PTSD and traumatic stress regardless of comorbid BPD is limited.
Current Study
Aims
• Understand how DBT treatment can positively impact PTSD symptoms
• Add to body of literature on alternative applications of DBT to traumatic stress profiles distinct from BPD-related trauma presentations
Hypotheses
• Significant reductions in all PTSD symptom clusters
• Greater change in PTSD symptom severity realized with more time in DBT treatment
Method
Participants
Clients enrolled in standard 6 or 12-month DBT program in a outpatient private practice and training institute July 2017 and May 2018 who had completed at least two intervals of the clinical assessment battery that included the PCL-5 were included in the study (n = 21). 66.7% of participants are female with mean age of 30.73 years (SD = 11.64). 61.9% sought DBT treatment without BPD diagnosis. Mean time in treatment as a function of interval between PCL-5 assessments was 109.86 days (SD = 50.29)
Measures
The PCL-5 is a 20-item self-report measure of PTSD symptom severity 5 as defined by the DSM-5. Symptom subscales include re-experiencing and emotional distress (Criteria B), avoidance (Criteria C), negative thoughts or feelings (Criteria D) and hyperarousal and self-destructive behavior (Criteria E).
Time in treatment was measured as an interval of total days between initial and most recent PCL-5 measure completion due to rolling DBT program enrollment.
Procedure
Participants received treatment in a standard DBT program that included DBT Skills Training Modules, individual psychotherapy, telephone coaching and consultation and completed intake and secondary clinical assessments
Data Analysis
A pretest-posttest design was used to analyze the effects of DBT on PTSD symptomatology. Nonparametric Wilcoxon Signed Ranks Test was used differences between initial and post-treatment interval PCL-5 total and subscale scores.
To assess relationships between time in treatment and change in PTSD symptomatology, Spearman’s rho correlations analyzed days in treatment and PCL-5 overall and subscale score changes.
Results
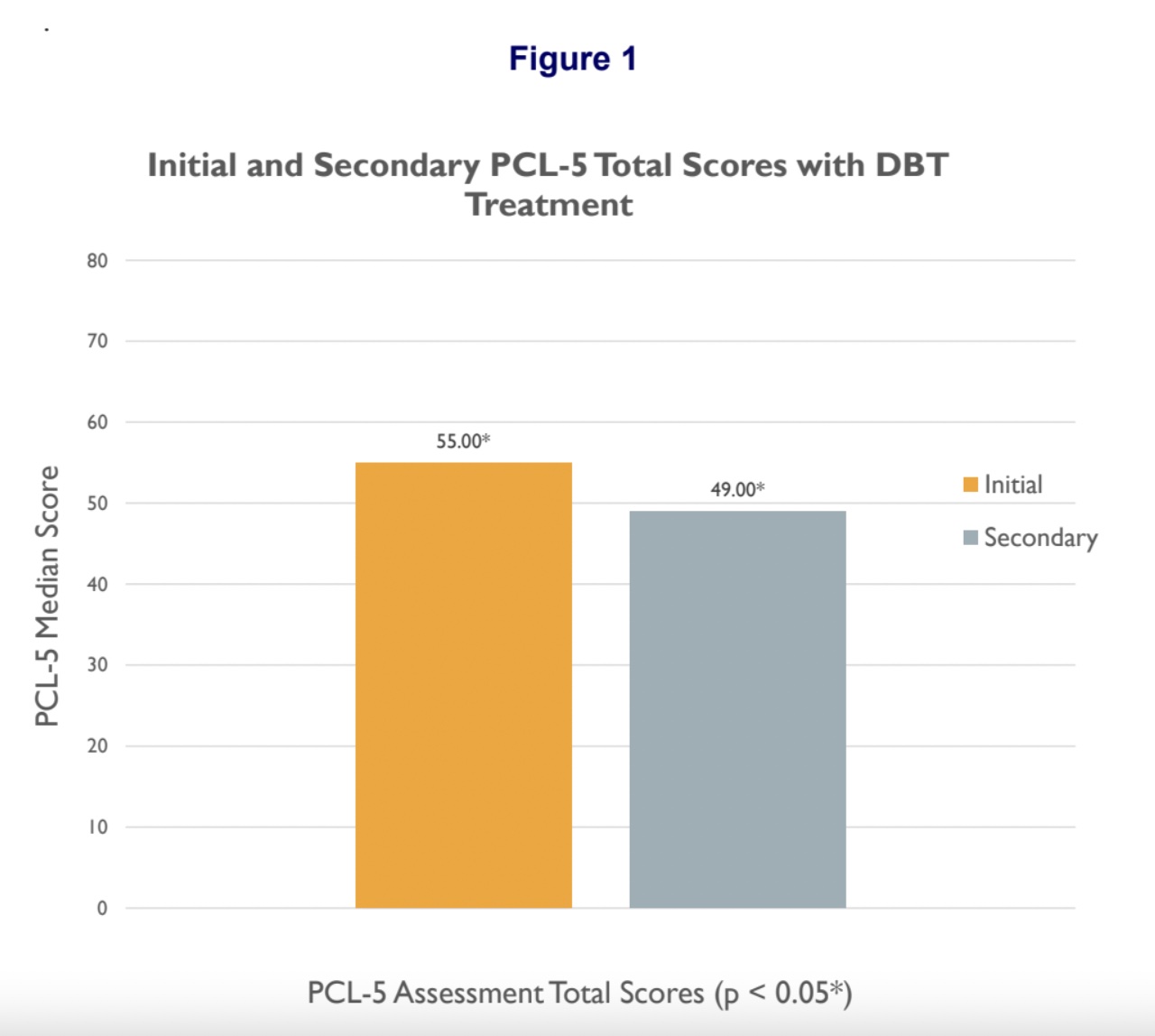
- Secondary total PCL-5 scores (Mdn = 49) were significantly lower than initial PCL-5 total scores (Mdn = 55), Z = -2.260, p = .024.
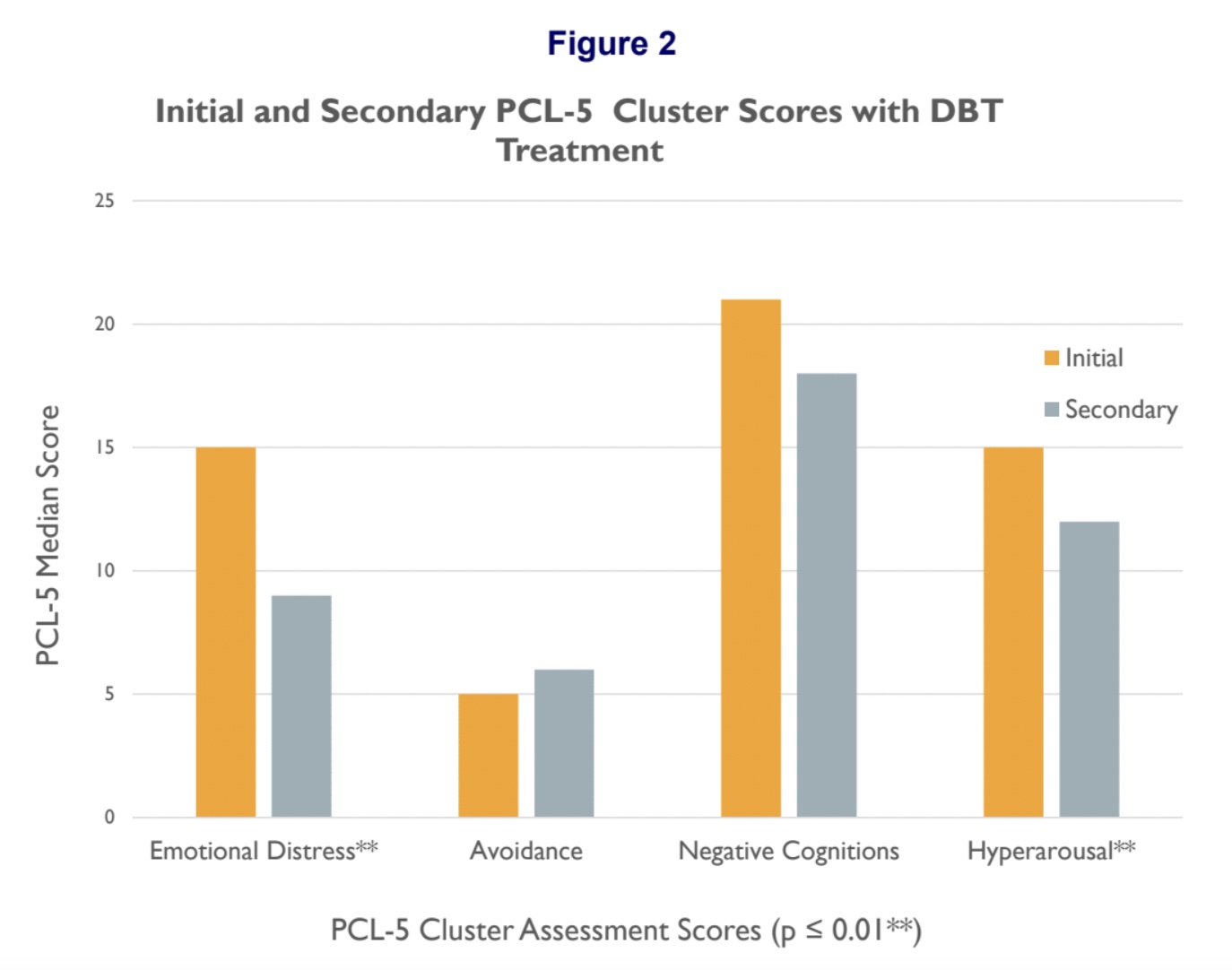
- Significant reductions were found in Criteria B (Mdn = 9), Z = -2.662, p = .008 and Criteria E subscale secondary scores (Mdn = 12), Z = -2.514, p = .012.
- No significant differences in secondary Criteria C (z = -.286, p = .775) or Criteria D (Z = -1.394, p = .163) subscales were found.
- Time in DBT treatment was positively related to change in total PCL-5 score (r (21) = .385, p= .05), but was not related to changes in PTSD criteria subscales
- PCL-5 total score change was positively related to all subscales at the p = .01 level.
Discussion
- Trauma-related emotional distress, hyperarousal and self-destructive behavior found to be significantly reduced with DBT treatment; PTSD-related negative cognitions and avoidance not significantly different
- Continued DBT treatment related to greater changes in overall PTSD presentation, which related to greater changes in each PTSD symptom cluster
- Findings consistent with DBT goals of reducing emotional dysregulation and self- destruction which severely limit psychosocial functioning; may show how DBT prepares clients to address trauma once emotionally and behaviorally stabilized, or which PTSD profiles are DBT-responsive
- Future research into specific DBT components, treatment settings and impacts on varied presentations of PTSD with non-BPD comorbidity (e.g.: anxiety, depression or substance use disorders) needed
Research conducted by: Carol M. Lazo, M.B.A., Marget C. Thomas, Psy.D., Max Stivers, B.A., Rob Montgomery, B.F.A., Molly Moffit, B.A., Lynn McFarr, Ph.D.
References
1. Bradley, R., Greene, J., Russ, E., Dutra, L., and Westen, D (2005) A multidimensional meta-analysis of psychotherapy for PTSD. American Journal of Psychiatry, 16 (2), 214 – 227.
2. Bohus, M., Dyer, A.S., Priebe, K., Kruger, A., Klenidienst, N., Schmahl, C., Niedtfeld, I., and Steil, R. (2012). Dialectical behavior therapy for Post-Traumatic Stress Disorder after Childhood Sexual Abuse in patients with and without Borderline Personality Disorder: A randomized controlled trial. Psychotherapy and Psychosomatics, 82, 221 – 233.
3. Harned, M. (2012) Integrating Treatment for PTSD into Dialectical Behavior Therapy for Borderline Personality Disorder [PowerPoint Slides].
4. Wagner, A.W., Rizvi, S. L., and Harned, M.S. (2007). Applications of dialectical behavioral therapy to the treatment of Complex Trauma-Related problems: When one case formulation does not fit all. Journal of Traumatic Stress, 20 (4), 391 – 400.
5.Weathers, F.W., Litz, B.T., Keane, T.M., Palmieri, P.A., Marx, B.P., & Schnurr, P.P. (2013). The PTSD Checklist for DSM-5 (PCL-5). The National Center for PTSD.

