Background
• Serious Mental Illness (SMI): One or more mental disorder diagnoses along with impaired functioning of daily activities, including frequency of suicidal ideation, attempts, and/or hospitalization. [1]
• Dialectical Behavioral Therapy (DBT) treatment is highly effective amongst people with mental disorders involving emotional dysregulation. [2]
• Existing research has yet to explore the relationship between different kinds of SMI and treatment outcomes. [3]
Present Study
Aim: This study examines the association between SMI and treatment outcomes in DBT.
• Hypothesis: Those with SMI would experience lower improvement rates in treatment outcomes compared to those without SMI.
Participants
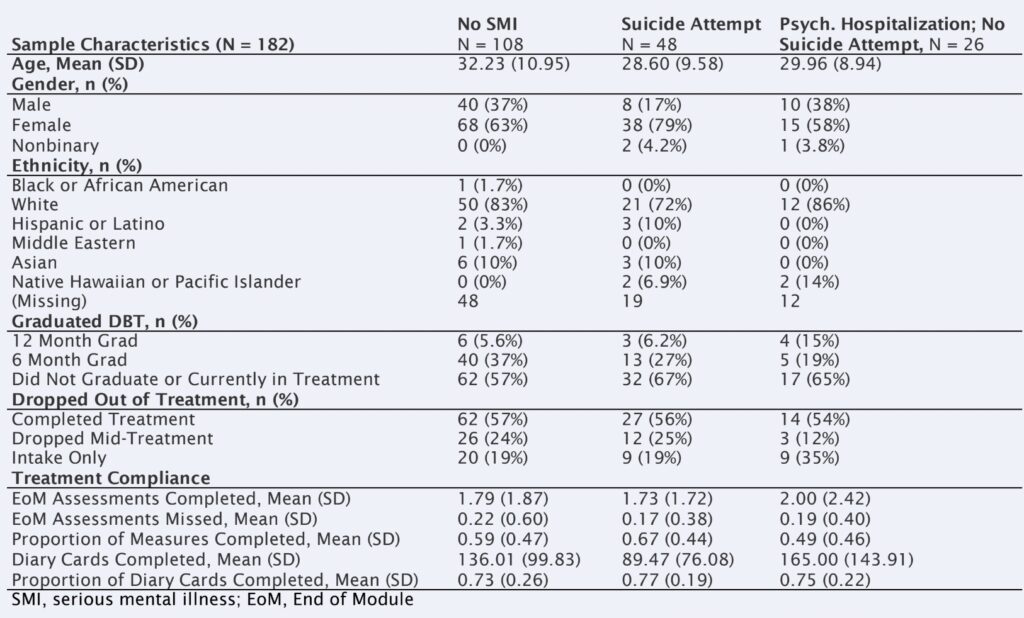
• N= 182; 66% female; mean age 30.95. Patients completed comprehensive DBT treatment at an outpatient clinic and training center in California.
➔ Grouped as follows:
○ those with previous suicide attempt (n = 48)
○ those with previous hospitalization, but no suicide attempt (n = 26)
○ those who had neither (n = 108)
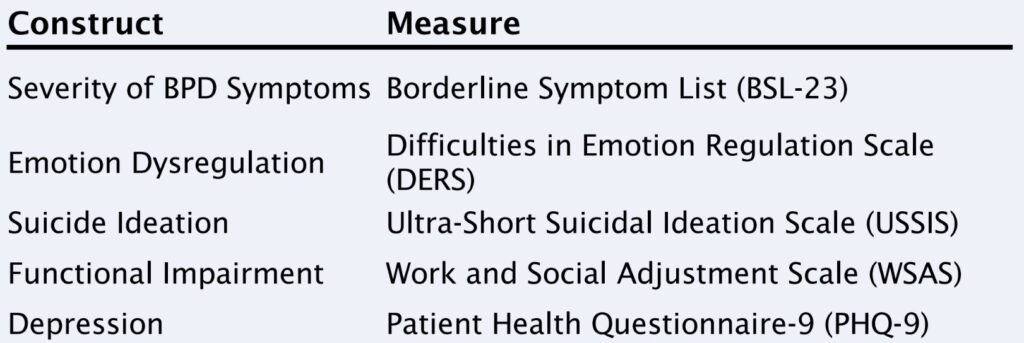
Measures
• Outcome measures used: BSL, DERS, USSIS, WSAS, and PHQ-9
• Participants completed outcome measures at intake and every 2 months throughout DBT treatment
Method
• Multilevel modeling was used to examine the trajectory of changes in outcome measures over the course of treatment.
Results
• Results indicated that the presence of SMI at intake was associated with greater baseline severity of all outcomes (ps< .05), except the DERS-18 (p =.133). Also, for the USSIS the interaction between SMI and time in treatment was statistically significant (p < .001). This indicates that individuals with SMI improved at a faster rate than those without SMI.
• Our hypothesis was not supported: Those with SMI reported more severe symptoms at baseline, but there was no statistically significant difference in the rate of improvement between groups for all outcomes with the exception of suicidality.
Discusion
•Those with SMI improved at the same rate as those without SMI except with regards to suicidality where those with SMI improved three times faster.
• Participants with SMI were not significantly more emotionally dysregulated at baseline based on the DERS-18, but all other measures showed significant differences between between groups.
Strengths
○ Real world outpatient sample
○ Use of multiple scales to track symptoms over time
○ Measures given multiple times during treatment
Limitations
○ No control group
○ Small sample size of clients with SM
Future research
○ Assess whether expanded definitions of SMI uniquely predict treatment outcomes
○ Assess outcomes among those with SMI completing DBT in different treatment settings
Research conducted by: Augusta Bolwell, Psy.D., Sydney Ramsey, B.A, Saad Iqbal, B.A., Tonia De Barros Barreto Morton, B.A., Robert Montgomery, M.A., & Lynn McFarr, PhD
References
[1] Neacsiu,A.D., Eberle,J.W., Kramer,R.,Wiesmann, T.,&Linehan,M.M.(2014).Dialectical behavior therapy skills for trans diagnostic emotion dysregulation: a pilot randomized controlled trial. Behaviour research and therapy, 59,40–51. https://doi.org/10.1016/j.brat.2014.05.005
[2] Sahin,Z., Vinnars,B.,Gorman, B.S.,Wilczek,A., Åsberg,M., & Barber,J.P.(2018). Clinical severity as a moderator of outcome in psychodynamic and dialectical behavior therapies for borderline personality disorder. Personality disorders,9(5), 437–446. https://doi.org/10.1037/per0000276
[3] Wasser,T., Tyler,R., McIlhaney,K., Taplin,R., &Henderson,L.(2008). Effectiveness of Dialectical Behavior Therapy (DBT) versus Standard Therapeutic Milieu (STM )in a Cohort of Adolescents Receiving Residential Treatment. Best Practice in Mental Health, 4(2), 114–125.

