Background
- PTSD and BPD are frequently comorbid disorders that are associated with a history of trauma, but their relationship is not well understood. They have a comorbidity rate of 25-55.9% (Jowett et al., 2020).
- DBT is found to reduce symptoms of BPD and PTSD.
- Higher levels of self-reported skill use in DBT treatment was found to be associated with decreased emotional distress and more positive treatment outcomes.
- Skills homework completion was significantly associated with a reduction in urges for suicidal behaviors and substance use.
- New research is needed to understand the relationship between specific DBT interventions and symptom reduction in comorbid BPD and PTSD.
Present Study
This study will examine effect of diary card completion on BPD and PTSD comorbid symptoms and improvement in emotional regulation.
Hypotheses:
H 1: Symptoms of PTSD and BPD will decrease over the course of treatment.
H 2: Symptoms of PTSD and BPD will decrease over the course of treatment along with with diary card completion.
 Methods
Methods
● Participants (n = 299, M age = 27.9, SD = 11.3; 65% Female, 31% Male, 4% Nonbinary or Transgender) were patients completing comprehensive DBT treatment at an outpatient clinic in Southern California.
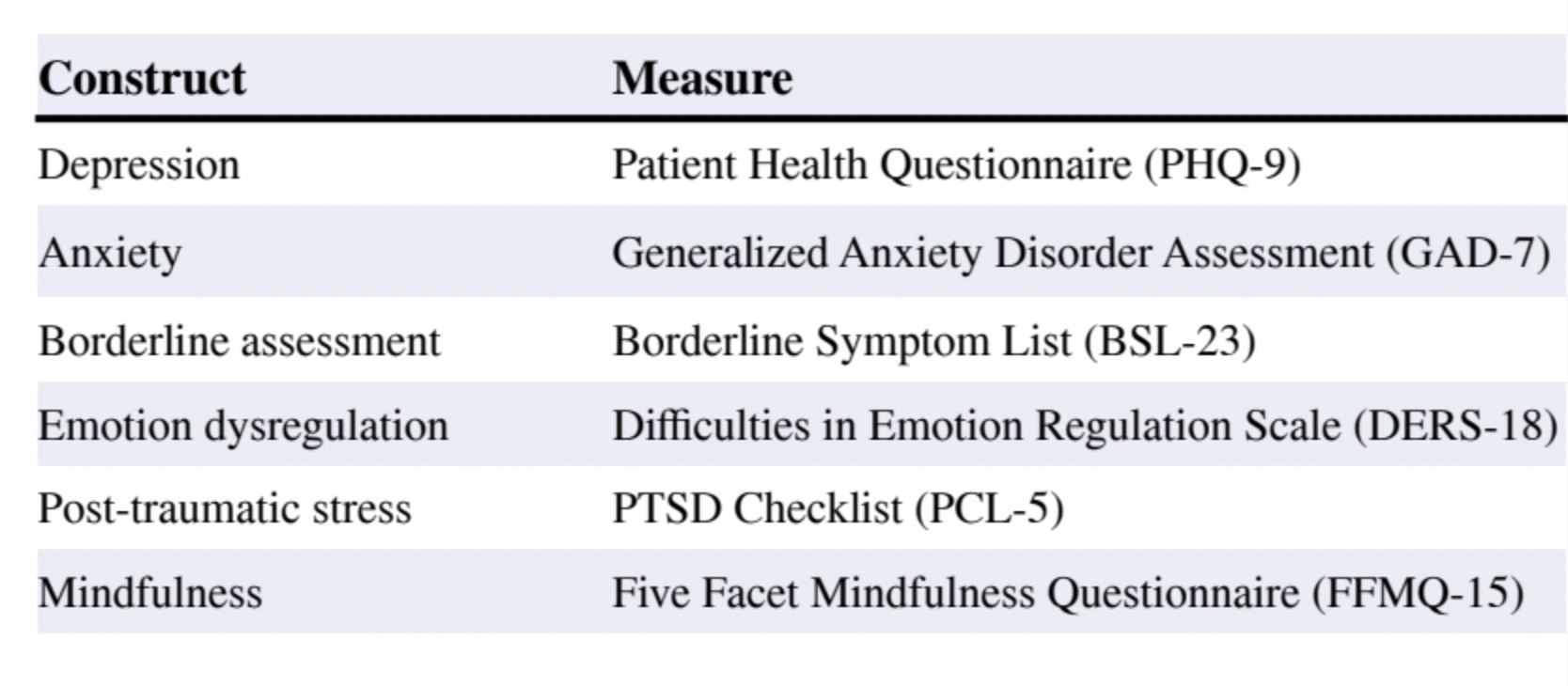
● Measures included the PHQ-9, GAD-7, BSL-23, DERS-18, PCL-5, and FFMQ-15, and were collected at intake and every 2 months throughout treatment. Diary card data was collected daily.
● Data analyses were conducted using R Studio. Mixed Linear Effects Models were used to examine the association between diary card completion and change over time in outcomes.
● Time in months from baseline, the proportion of diary cards completed (ranging from 0 to 1), and the interaction between the two were included in the final model for each outcome.
Results
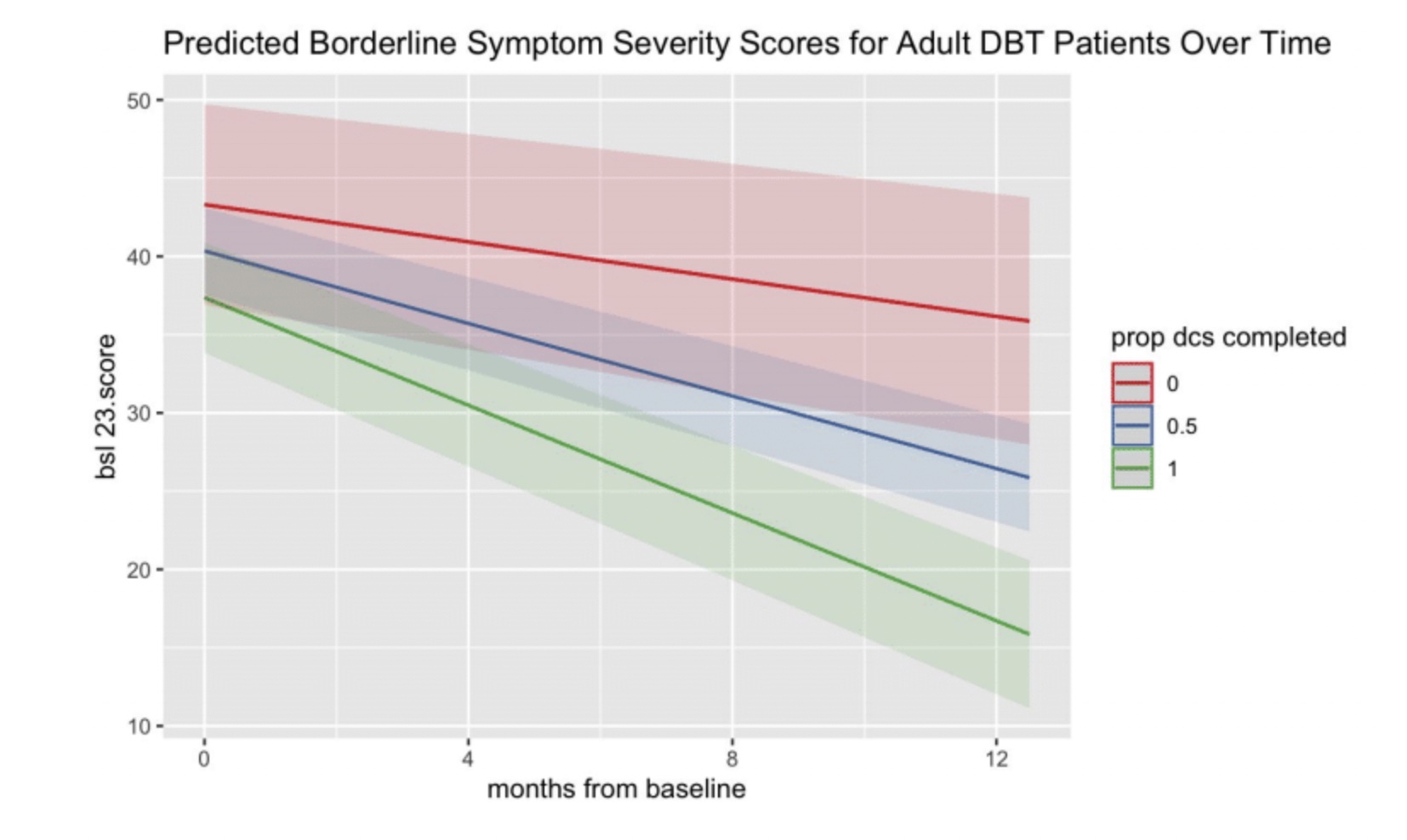
● Significant interactions between months in treatment and diary card completion rate were found for PHQ-9, GAD-7, and BSL-23 (highest significance); the higher the proportion of diary cards completed by a patient, the greater their improvement for each month of treatment
● Interaction effects for the DERS-18 (b = -.49, se = .26, p = .062), PCL-5 (b = -.72, se = .40, p = .080), and FFMQ-15 (b = .30, se = .20, p = .129) were nonsignificant, though were directionally the same as the other effects
Discussion
The primary hypothesis was partially supported: greater diary card completion was associated with rapid improvement in symptoms of depression, anxiety, and BPD; however, this relationship was weak to nonexistent for emotion dysregulation, trauma symptoms, and trait mindfulness. The results of this study suggests that although there were significant improvements on some scales, the other scales evaluated may not be statistically significant due to varied patient engagement, severe PTSD symptoms being an obstacle to consistent diary card completion, or error given that these are self-report measures. Further research is needed to understand the effects of diary card completion and duration of treatment on PTSD, trait mindfulness, and emotion regulation.
Strengths
● Real world, outpatient sample.
● Use of multiple scales to track treatment over time.
● Measures collected regularly throughout treatment.
Limitations
● Limited generalizability to full model DBT treatment and lack of control group.
● Adherence to diary card completion could be inconsistent based on variability in therapy interfering behaviors amongst therapists.
● Treatment may have differed between new and more experienced clinicians.
Future research
● Considering why some symptoms were highly correlated with diary card completion was outside of the scope of this study, but may be an exciting topic for future research.
Research conducted by: Lily Sakhan, M.A., Courtney Maliakkal, M.A., Cassandra Lloyd, M.S., Tonia De Barros Barreto Morton, B.A., Sydney Lopez, B.A., Robert Montgomery, M.A., Alexandra King, Ph.D., & Lynn McFarr, Ph.D.
References
[1] Choate, A., Fatimah, H., & Bornovalova, M. (2021). Comorbidity in borderline personality: understanding dynamics in development. Current Opinion in Psychology 37. 104-108.
[2] Jowett, S., Karatzias, T., & Albert, I. (2020). Multiple and interpersonal trauma are risk factors for both post‐traumatic stress disorder and borderline personality disorder: A systematic review on the traumatic backgrounds and clinical characteristics of comorbid post‐traumatic stress disorder/borderline personality disorder groups versus single‐disorder groups. Psychology and Psychotherapy, 93(3), 621–638.
[3] Roberts, N. P., Back, S. E., Mueser, K. T., & Murray, L. K. (2020). Treatment considerations for PTSD comorbidities. In D. Forbes, J. I. Bisson, C. M. Monson, & L. Berliner (Eds.), Effective treatments for PTSD: Practice guidelines from the International Society for Traumatic Stress Studies., 3rd ed. (pp. 417–450). The Guilford Press.
[4] Steil, R., Dittmann, C., Müller-Engelmann, M., Dyer, A., Maasch, A., & Priebe, K. (2018). Dialectical behaviour therapy for posttraumatic stress disorder related to childhood sexual abuse: a pilot study in an outpatient treatment setting. European journal of Psychotraumatology, 9(1). doi:10.1080/20008198.2018.1423832.

